Safer Sleep
Image credit: Sarah Conlan Lifestyle Photography
The key health promotion messages for safe infant sleep supported by Red Nose and the Australian Sleep Safe My Baby public health campaign are based on high-quality evidence [1, 10]:
Sleep baby on the back from birth, not on the tummy or side
Sleep baby with head and face uncovered
Keep baby smoke free before birth and after
Provide a safe sleeping environment night and day
Sleep baby in their own safe sleeping place in the same room as an adult caregiver for the first six to twelve months
Breastfeed baby
There are many resources to assist you in creating a safe infant sleep space consistent with the evidence that supports your baby to sleep safely in an environment consistent with their dynamically changing developmental needs. Several of these are provided at the conclusion of this article.
Sharing sleep with a baby
In providing a safe sleep environment night and day, and creating a baby’s own safe sleep place, we need to consider the location where baby is placed to sleep and the immediate environment in which baby is placed.
Room-sharing for the first 6-12 months remains an important risk reduction strategy for every family. Sleeping your baby in a separate room has been shown to increase the risk of sudden infant death threefold [6, 7, 8]
Creating a baby’s own safe sleeping place, which aims to protect their airway and minimise potential airway obstruction, is sometimes easier to create in a separate but adjacent sleep environment such as a cot or bassinet in the same room as the parent/s sleep. However, it is important to remember that no environment is risk-free for a baby as they dynamically develop during the first year of life; a cot or bassinet is only safe if is prepared for a baby to sleep in with infant safety in mind.
Credit: Red Nose Australia
Shared sleeping with a baby, often referred to as bed-sharing and/or co-sleeping, is an extremely common infant care practice, even in contemporary Western societies. Bed-sharing and co-sleeping are associated with many benefits [3, 4, 5] however the risk of sudden unexpected death in infancy including Sudden Infant Death Syndrome (SIDS) and fatal sleeping accidents is increased in certain circumstances [23, 6, 19, 20, 21].
A recent study from Queensland, Australia [11] was consistent with earlier findings from the United Kingdom [12], reporting approximately 76.9% of families have shared a sleep surface with their baby during the first three months of life, while half (49.6%) had shared a sleep surface in the last two weeks. For 1 in 5 babies (22%) this was for most or every night; 57.3% of parents reported that shared sleeping was not usually planned. These findings are consistent with previous studies in Australia with rates reported between 51-80% depending on infant age at the time of measurement [11, 18, 13, 14, 15, 16, 17]
This research strongly suggests that evidence-based information on how to share sleep with a baby more safely should be made available to all families regardless of original intentions given the likelihood that this practice will occur, whether intended or not, as parents respond to the needs of their baby in the context of their individual family circumstances.
“Strategies to make shared sleep safer are relevant for all families with young infants. Many parents will fall asleep with their baby whether they intend to, or not.”
Little Sparklers supports the risk minimisation approach to shared sleeping with a baby taken by Australia’s Red Nose organisation, our national peak body which promotes safe infant sleeping; the Australian Breastfeeding Association, and the Australian College of Midwives.
In addition, the United Kingdom’s Lullaby Trust and Basis- Baby Sleep Information Source promote strategies which support a risk minimisation approach.
Sharing the same sleep surface with a baby is a complex issue that encompasses many factors [19, 22]. A risk minimisation approach to shared sleeping considers the individual’s family’s circumstances when providing advice about infant care practices that parents will use in caring for their baby. In ensuring the safety of babies, it is crucial to respect and support family and cultural norms and practices [22, 10]).
Little Sparklers supports the promotion of consistent, evidence-based information to parents about the benefits, contraindications and strategies to enhance safety associated with shared sleep environments so that parents and carers can make informed decisions regarding sleeping arrangements for their baby that address their family circumstances and the dynamically changing needs of their baby [22, 19].
The benefits and risks of shared sleeping together with a comprehensive list of strategies to reduce risk for baby in shared sleep environments can be found in statements produced by:
These evidence-based sources also contain important information about infant, family and environmental factors that need consideration as you apply this information to your family circumstances.
In summary
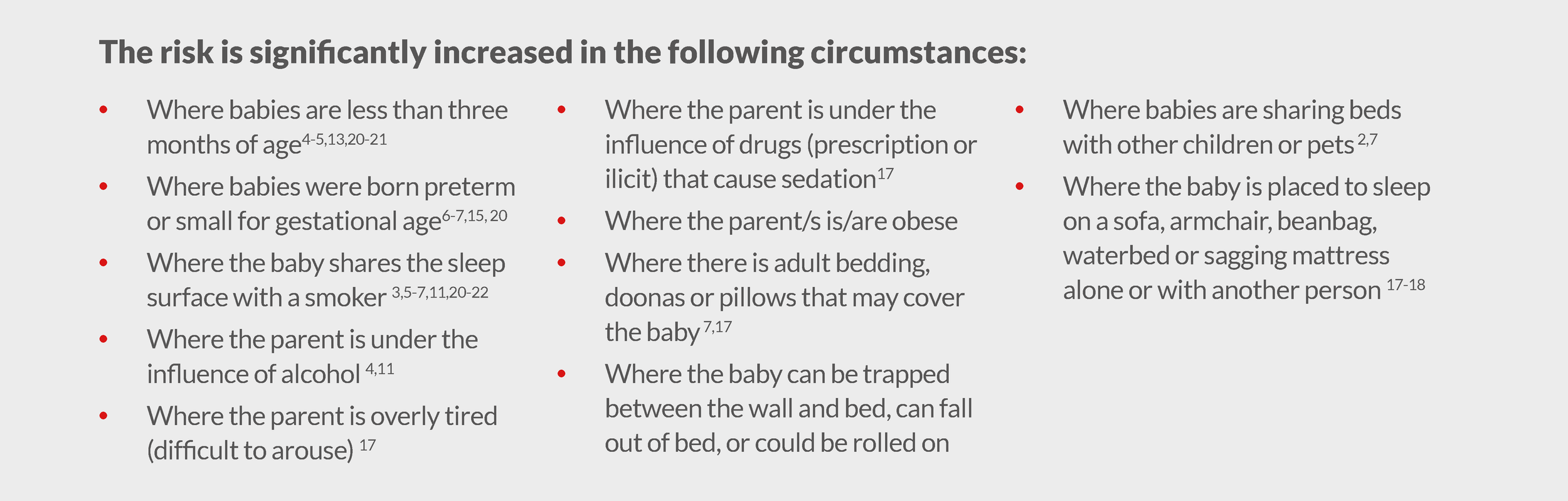
The risk of shared sleeping is significantly increased in the following circumstances:
[Reproduced with permission, Red Nose Information Statement ‘Sharing a Sleep Surface with a Baby’]
It is not safe to share a sleep surface with a baby if [22, 10]:
Either parent is a smoker
Either parent is under the influence of alcohol or illicit drugs
Either parent is under the influence of medication that causes sedation, is excessively tired, or obese.
Whether shared sleep is intended or not, the following strategies have been demonstrated to reduce the risk of sudden unexpected deaths in infancy, including SIDS and fatal sleeping accidents in shared sleeping situations [22, 10]:
Sleep baby on the back from birth – never on the tummy or side.
If baby lies on his or her side to breastfeed, baby should ideally be returned to the supine (back) position for sleep.
Make sure the mattress is firm and flat (not tilted or elevated)
Make sure that bedding cannot cover baby’s face or overheat baby (use lightweight blankets and remove pillows, doonas and other soft items from the environment that could cover baby);
Sleep baby beside one parent only, rather than between two parents, to reduce the likelihood of baby becoming covered by adult bedding (unless sleep enabler that provides for a separate sleep surface and infant bedding is being used)
Ensure partner knows baby is in the bed, if relevant to family circumstance
As an alternative to bedding, an infant sleeping bag may be used so that the baby does not share the adult bedding. (N.B. Do not wrap baby if sharing a sleep surface as this restricts arm and leg movement).
Make sure baby cannot fall off the bed. A safer alternative is to place the mattress on the floor (be aware of potential situations where baby can become trapped). Do not place pillows at the side of the baby to prevent rolling off.
Pushing the bed up against the wall can be hazardous. Babies have died after being trapped between the bed and the wall.
Avoid placing a baby to sleep in a bed with other children or pets
Remove teething necklaces from baby before sleep, if used
Babies must never be left alone on an adult bed or put to sleep on a sofa, bean bag, waterbed or soft, sagging mattress.
If baby is sleeping in a baby sling or baby carrier device use the TICKS principles for safe sling and carrier use to promote infant safety. In particular, ensure baby’s face is clear and can be observed and that baby is not in a curled chin to chest position that may cause airway compromise.
Three sided-cots (a cot with one side down) may be available for purchase that can be attached to the side of the bed at the same level so that the baby has a separate environment but is still in contact with a parent during sleep. Please note that currently there is no Australian standard for three-sided cots.
Key resources
This video created by Lullaby Trust and Basis is an excellent resource on how to cosleep more safely:
Contributed by: Professor Jeanine Young AM FACN, PhD, Bsc(Hons) Nursing (1st Class), Dip. Adv Nursing Care, RN RM Neonatal Nurse (ENB 405 Special and Intensive Care of the Newborn), Little Sparklers Director
REFERENCES:
[1] Young J, Watson K, Ellis L, Raven L. (2012) Responding to the evidence: Breastfeed baby if you can – the sixth public health recommendation to reduce the risk of sudden unexpected death in infancy. Breastfeeding Review 20(1): 7-15.
[2] Red Nose (2020a) Safe Sleeping: Six ways to sleep baby safely and reduce the risk of sudden unexpected death in infancy. Melbourne: Red Nose. Viewed 20 October 2020 at https://rednose.org.au/downloads/RN3356_Safe_Sleeping_Poster_A3%28web%29.pdf
[3] Ball HL. (2002) Reasons to bed-share : why parents sleep with their infants, Journal of reproductive and infant psychology, 20 (4):207-222.
[4] Ball HL. (2003) Breastfeeding, bed sharing and infant sleep. Birth. 30(3): 181-188.
[5] McKenna JJ, Ball HL, & Gettler LT. (2007) Mother-infant co-sleeping, breastfeeding and sudden infant death syndrome: What biological anthropology has discovered about normal infant sleep and pediatric sleep medicine. Yearbook of Physical Anthropology 50: 133-161.
[6] Blair PS, Fleming PJ, Smith IJ, Ward-Platt M, Young J, Nadin P, Berry PJ, Golding J and the CESDI SUDI Research Group. (1999) Babies sleeping with parents: case-control study of factors influencing the risk of the sudden infant death syndrome. British Medical Journal 319(7223): 1457-1462.
[7] Blair PS, Sidebotham P, Berry PJ, Evans M, Fleming PJ. (2006) Major epidemiological changes in sudden infant death syndrome: a 20 year population-based study in the UK. The Lancet 367(9507): 314-319.
[8] Moon RY, Horne RS, Hauck FR (2007) Sudden infant death syndrome. Lancet 370(9598):1578-89.
[9] Red Nose. National Scientific Advisory Group (2020b) Information Statement: Room-sharing. [First posted October 2008, recently updated December 2016]. Melbourne: Red Nose, National SIDS Council of Australia. http://www.rednose.org.au
[10] Red Nose. National Scientific Advisory Group (2020c) Information Statement: Sharing a sleep surface with a baby. [First posted February 2006 recently updated December 2019]. Melbourne: Red Nose, National SIDS Council of Australia. http://www.rednose.org.au
[11] Cole R, Young J, Kearney L, Thompson JMD. (2020) Infant care practices and parent uptake of safe sleep messages: a cross-sectional survey in Queensland, Australia. BMC Pediatrics 20(27) https://doi.org/10.1186/s12887-020-1917-5
[12] Lullaby Trust (2019) New survey shows 405 of parents are not co-sleeping safely. Available 21 October 2020 at https://www.lullabytrust.org.uk/new-survey-shows-40-of-parents-are-not-co-sleeping-safely/
[13] Rigda RS, McMillen IC, Buckley P (2000) Bed sharing patterns in a cohort of Australian infants during the first six months after birth. Journal of Paediatrics and Child Health 36(3): 181-188.
[14] Panaretto KS, Smallwood VE, Cole P, Elston J, Whitehall JS. (2002) Sudden infant death syndrome risk factors in north Queensland: A survey of infant-care practices in Indigenous and non-Indigenous women. Journal of Paediatrics and Child Health 38(2): 129-134.
[15] Schluter PJ, Young J. (2002) Reducing the risk of Sudden Infant Death Syndrome: what infant care practices are being used by primary care-givers in Queensland? Neonatal, Paediatric and Child Health Nursing 5(2): 27-35.
[16] Young J, Battistutta D, O'Rourke P, Thompson JMD. (2008). Infant Care Practices Related to Sudden Infant Death Syndrome in Queensland 2002. Brisbane: Queensland Health.
[17] Young J, Thompson J. (2009). Recommendations for real life: the nature of shared sleep environments in Queensland and implication for effective safe infant sleeping messages. Forensic Science, Medicine and Pathology, 5(2): 115.
[18] Cunningham HM, Vally H, Bugeja L. (2018) Bed-sharing in the first 8 weeks of life: An Australian study. Maternal and Child Health 22(4): 556-564. doi: 10.1007/s10995-017-2424-7.
[19] Young J, Shipstone R. (2018) Shared Sleeping Surfaces and Dangerous Sleeping Environments [Chapter 11]. In BYARD RW, DUNCAN J. (Eds.) SIDS, Sudden Infant and Early Childhood Death: The Past, The Present and the Future. 1st ed. Adelaide: University of Adelaide Press. Available at https://www.adelaide.edu.au/press/titles/sids/sids-ebook.pdf
[20] Shipstone R, Young J, Thompson JMD. (2019) The real divide: the use of algorithm-derived Indigenous status to measure disparities in sudden unexpected deaths in infancy in Queensland. Australian and New Zealand Journal of Public Health Online; http://doi: 10.1111/1753-6405.12951. (Published 31 October 2019).
[21] Shipstone R, Young J, Kearney L, Thompson JMD. (2020) Applying a social exclusion framework to explore the relationship between Sudden Unexpected Deaths in Infancy (SUDI) and social vulnerability. Frontiers in Public Health (Inequalities in Health) https://www.frontiersin.org/articles/10.3389/fpubh.2020.563573
[22] Australian College of Midwives (2014) Co-sleeping and Bed-sharing (ACM) Position Statement - 2014. Position Statement on Bed-sharing and Co-sleeping. [Published Nov 2014]. Canberra: Australian College of Midwives (Dr J. Young, Acknowledged Author). https://www.midwives.org.au/resources/co-sleeping-and-bed-sharing-acm-position-statement-2014
[23] Bartick, M., Tomori, C. (2019). Sudden infant death and social justice: A syndemics approach. Maternal and Child Nutrition, 15, e12652. https://doi.org/10.1111/mcn.12652